1: Where does it all go?
The NHS Five Year Forward View outlines generic principles that are expected to govern UK’s healthcare system by 2020/21 [1]. The report was published in October 2014 and we are getting close to the mid-way point of the 5-year plan.
The report predicts that there will be a steady increase in Healthcare operational costs and that these costs will result in £30Bn deficit in healthcare funding by 2020/21. As a result, the report evaluates different ways to introduce efficiencies into the current system and proposes new funding models.
At present hospital related services are paid by the NHS based on the actual work-load that is reported and budgeted by hospitals. On the other hand, GP practices are funded on patient lists, i.e. headcount. In short, this means that hospitals receive funds per visit/encounter, whereas GP’s are funded per person regardless of how many visits/encounters the individual has to the practice.
Although there’s not a very clear transparency on how much funding hospitals receive out of £100+Bn annual NHS budget, the figures are likely between £50-£60Bn, while GP’s receive £6.7Bn.
It is no surprise that under the Five Year Forward View experts are suggesting a wider distribution of healthcare provisioning, which means moving more work from hospitals to the local community. Effectively, this move will add more workload to GP’s and other primary care services. Under this model, GP’s are being envisaged as multispecialty community providers transforming into heterogenous practices bringing in senior nurses, consultant physicians, geriatricians, pediatricians, and psychiatrists to work alongside community nurses, therapists, pharmacists, psychologists, social workers, and other staff. All this should alleviate the influx of patients into hospitals.
This in turn will have clear implications for GP practices going forward:
- Considering the shortage of the health professionals entering the sector as GPs and the increasing number of GP’s who plan to leave the sector, it is likely there will be little to no increase in the number of practicing GPs; the current increase is around 0% to 1% annually [2]. This hardly compensates for the changes in demographics and further still does not compensate for the re-distribution of patients to local community. Hence, existing GP’s will have to cope with higher number of patients. At present the average number of patients on a GP list is 1,800 and a single GP can have between 40-60 patient contacts per day;
- The number of visits to GP’s has increased from on average 3 times a year to 6 times a year in the last decade. Due to the UKs increasing older population it can be expected the annual number of visits will climb further;
- Older patients require typically more time for consultation than the minimum 10 minutes set aside for a single meeting. This in turn will put pressure on the number of patient contacts a GP can make in the future;
- With an increasing older population, the number of people requiring either home visits or nursing home visits will increase – which in turn means the time a GP spends travelling to see patients could increase significantly. Time spent travelling is time that will be taken away from GPs to actually have contact with patients.
All in all, the GP role is becoming more prominent in the healthcare sector, however, the practices will also face further challenges with regards to time pressure.
While technology is not a panacea, it could be speculated that the health sector has yet to fully utilise the potential of certain technologies that are now becoming more mainstream. Certain technologies, if implemented correctly, would increase productivity in both primary and secondary care.
2: A Day in a GP practice
Lets take a few concrete examples from GP practices. The first one outlines the inefficiencies that may arise from communication barriers, whereas the second highlights the inefficiencies associated with home visits.
09.00: Call patient on display board and over the tannoy.
09.01: Patient finally arrives after GP has intercepted them walking down the wrong corridor. She has come alone and speaks no English, so Bengali interpreter needs to be organised.
09.03: Interpreter arrives after finishing with last GP. There is no Bengali interpreter available today so she will attempt to consult in Hindi or Urdu.
09.04: Interpreter reports that patient’s communication in Hindi/Urdu is limited so there’s no option to proceed.
09.06: Get through to Bengali interpreter on the phone, via Big Word.
09.09: Get a history of postmenopausal bleeding for the last three months.
09.10: Beeeeeeeeeeeeeeeeep! Time’s up. In effect, the time is not up, as the patient requires care and hence the session turns out to be 16 minutes in total as opposed to 10 minutes.
3: Where does the technology come into play and how can it help?
Did this encounter actually require a face to face visit? Likely no. The meeting could have been scheduled on video visitation system starting at 9am involving Bengali interpreter in three party video call. Remember, the GP is being paid by the number of patients on the list, and the more efficiently communication can be organised with the patients in need, the GP has the potential to see/support more patients or, the GP could manage a smaller cost base maintaining the same number of patients.
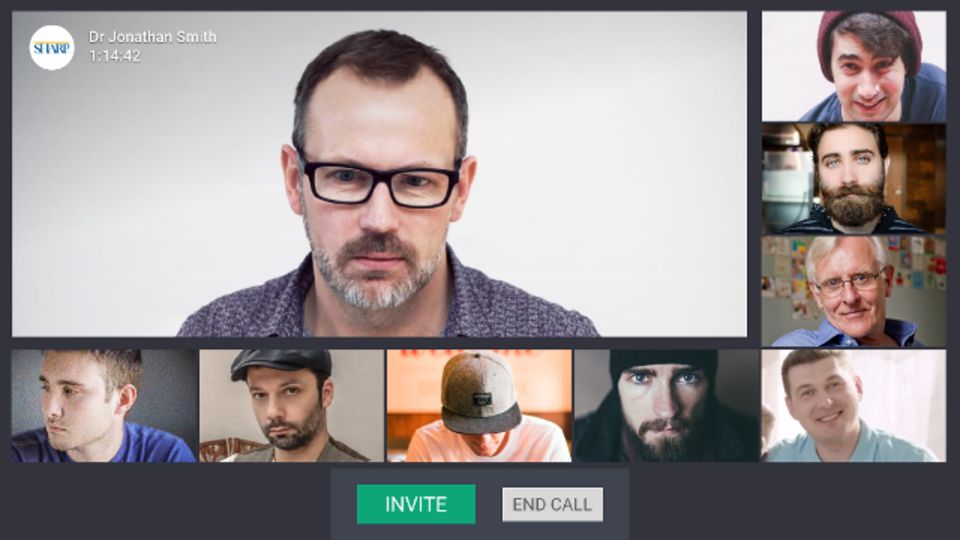
Now, let’s consider the financial implications. It is estimated that up to a whopping 80% of GP meetings could be done using video visitation tools [3]. In case these meetings can be done remotely, we see the following efficiencies to be introduced:
- Average patient travel time and waiting time is around 60 minutes. This is equivalent to a productivity cost of between £20-£30 for a single member of the public visiting the GP. In a month, the social cost of wasted time on travel alone could be reduced by £21,120 per GP;
- More efficient meeting time – each tele-consultation session can potentially save 2-3 minutes per visitor that otherwise is spent on waiting until the patient comes to the GPS office. It is all too often that due to transportation delays a patient may arrive late to a meeting causing unnecessary delays and wasted time for the GP. If on average, per day the savings from the meetings account for 90 minutes, a GP can meet with 8-9 more patients more a day. Given that the average remuneration per patient on the list is £136 and GP could add 340 more patients to its list (given on average 7 visits per year per patient) and charge extra £46,240 per GP to the NHS.
The outcome is more drastic if a GP also has to care for home-bound patients. It may be a nursing home with multiple patients or a private individual with limited mobility. It is estimated that around 40% of such visits could be done remotely. This means that on average a GP could serve 6-8 more people per home visit if home visits were replaced by video calls. If the number of such visits per month is 15, then in about 6 cases it could have been done remotely. The opportunity cost for it is 36-48 visits per month that could have been arranged at the practice.
Obviously, these figures are illustrative and do not present the absolute truth. However, with these examples we can see that achieving an efficiency increase of 15-20% is possible with technologies/tools that are widely available today. There are further reaching imprecations for the public; time spent commuting could be use more productive activities.
There are a few questions that could be raised regarding tele-conferencing;
- What is the return on investment for GPs by using suggested efficiencies?
- Why not simply use a traditional phone call?
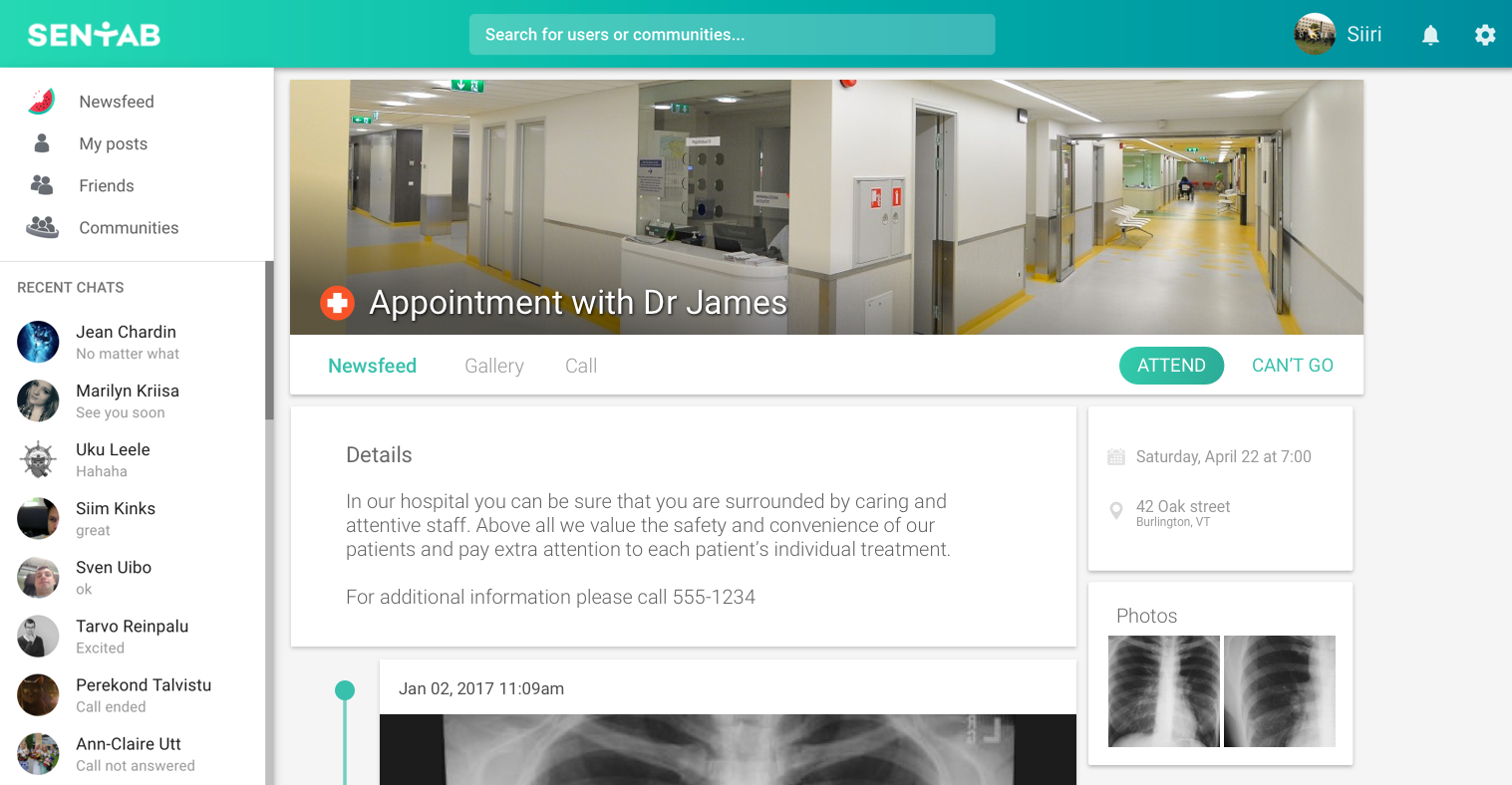
The good news is that Sentab supports multiple platforms, more specifically it can be used on a standard flat screen TV set. This facilitates and easy-to-access approach to people who do not own a smartphone, tablet, or laptop. The next requirement, the internet, is becoming more of a commodity in the UK and many residents have it as standard. By investing £115 into a InTouchTV box, you can reach several patients who may be considered more difficult to reach via modern communication methods. Given the small cost of a InTouchTV unit it is quite evident the return on investment for a GP will be seen within a very short space of time.
Regular phone calls are good for occasional conversations, however typically a) the situation calls for a visual inspection be it a general looks of a patient or the situation at his/her premises; b) more than 65% of people prefer to have video conversation with the doctor, as the time for the conversation is limited and information exchange will be more valuable if the voice is accompanied by actual visual interaction.
References:
[1] NHS. Five Year Forward View: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
[2] Kings Fund. https://www.kingsfund.org.uk/time-to-think-differently/trends/professional-attitudes-and-workforce/medical-workforce#gps